Products and Technologies
Inhalation Therapy For Alveolar Deposition
Technology Cluster
Pulmonary hypertension can be primary or secondary to a number of lung diseases. Primary pulmonary hypertension has no successful treatment and ultimately leads to mortality. Secondary pulmonary hypertension usually complicates a number of diseases that lead to alveolar hypoxia. The present medical management appears inadequate to meet the challenge of this common and frequently a fatal or uncontrolled problem.
One of the main treatment modalities for pulmonary hypertension is systemic delivery of vasodilators. The aim is to attempt to dilate the pulmonary blood vessels by giving the drug orally or by injection. Drugs like prazocin, nifedipine, phentolamine and sildenafin are among the variety of drugs tried for the purpose.
The systemic delivery requires high dosage in the circulation for the desired effect. The drug is distributed throughout the body fluids, but beneficial effect is limited to the target organ micro-vasculature of the lungs. The very high dosage has serious side effects like low blood pressure, significant palpitation and heart problems that limits the use of this treatment. This form of treatment is limited to serious cases at the most for a few days or weeks though most of the diseases, with which pulmonary hypertension is associated, are chronic and mild in nature and may require treatment for years or even for life. Also, there may not be any benefit at all if regional blood supply is blocked significantly due to thrombosis in the lung microvasculature. Systemic vasodilators are therefore, now considered an inadequate treatment in pulmonary hypertension but continue to be given in absence of a better treatment choice.
Other methods of treatment for pulmonary hypertension include oxygen inhalation (with or without 5 per cent CO2), Nitric Oxide inhalation therapy, and compressed/hyperbaric air administration. However, these therapies can only be given for short periods in time of emergency and are not suitable for prolonged continuous use. Secondly, the methods are costly and mostly require infrastructural facilities. Thirdly, they almost immobilise the patient for the period of therapy. Thus, though highly effective, these are useful only as hospital-based treatment for a short period.
Local acting particulate aerosols have not been used for treating pulmonary hypertension clinically. The main cause of this has been the inability of the commercially available aerosol/nebuliser/dispersion systems to deliver pharmacological dose to the pulmonary level. These systems are designed to act at bronchi-trachea level and are not useful for managing pulmonary hypertension.
Apart from pulmonary hypertension, many other diseases affect pulmonary tissue. These include widespread infection (viral or bacterial or fungal), acute inflammations (diffuse bronchiolitis/alveolitis/ ARDS/allergic conditions) or chronic inflammations (all lung conditions leading to fibrotic changes such as interstitial lung diseases and cancers). All these require higher concentration of drugs like antibiotics, antiviral substances, steroids, detergent/surfactants and anticancer drugs in the local space as compared to other tissues to enhance pharmacological effect as also to lower down the side effects. For the same reasons, systemic route and routine inhalation therapy is inadequate to meet the challenge though both continue to be used in absence of the better alternative.
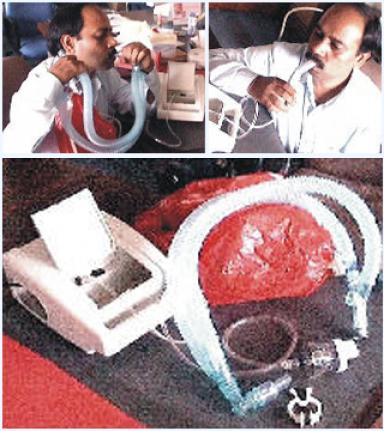
DRDO has developed a new treatment concept and methodology, called Inhalation Therapy for Alveolar Deposition (ITAD), for treating or preventing pulmonary hypertension and other pulmonary diseases. Considering the widespread and fatal or incapacitating nature of the diseases, and further considering the inadequacy of the present line of management with respect to control or cure, side effects, cost-effectiveness, and patient comfort, ITAD will be effective in control of these diseases and their symptoms and complications. It is also cost-effective, non-hazardous, capable of being used with minimal infrastructure needs, and easy to perform at field level.
In view of the inadequacies of the current inhalation systems used for alveolar deposition of other local acting or systemically acting drugs, DRDO has also developed a new strategy for depositing a higher amount of drug in the alveolar space for better pharmacological action with lower dose and lower side effects.
ITAD is a complete drug-delivery apparatus that upon combination with an air compressor and a nebuliser can be used for prevention or treatment either independently or concurrently with other treatments. It makes a complete disclosure of the drug-delivery apparatus that increases the deposition of the drug delivered in the pulmonary parenchyma enhancing the local pharmacological effect. It also increases the oxygen transport to the blood from the alveolar space.
Salient Features
Besides pulmonary hypertension, ITAD is also beneficial in a number of lung and chronic obstructive airway diseases like bronchial asthma, diffuse tuberculosis, emphysema, interstitial lung diseases, adult respiratory distress syndrome, and pulmonary edema.
Also beneficial in management of a special type of secondary pulmonary hypertensions like high altitude hypoxic hypoxemia, acute and chronic mountain sickness, high altitude pulmonary edema.
Pharmacological effects are higher and systemic side effects are less due to higher local deposition and lower systemic dose. Upon nebulisation and inhalation, the nebulised drug is preferably delivered to the peripheral lung parenchyma, evading significant deposition in oropharynx, trachea, and stomach. These drugs include steroids, surfactants, antibiotics, and antiviral amongst others.
Cost-effective.